Count Down to the Future – Meg Cheng-Campbell, Ryan T. Scott, Samantha Torres, Matthew Murray, Eric Moyer – NASA Ames Research Center
Oct 3, 2017biology, health and medicine, physical sciences
At the NASA Ames Research Center in California, the next generation of space biologists are working to understand the effects of long duration space flight on model organisms, and are developing ways to protect the health of future astronauts.

You may also like …

Dr. Rasha Bayoumi | Decolonizing Global Collaboration: Building Equitable Science Diplomacy
Science diplomacy, meaning the use of scientific collaboration to strengthen international relations and address shared global challenges, has long been hailed as a force for good. Yet, as Dr. Rasha Bayoumi of the University of Birmingham Dubai and her colleagues argue in their Editorial for a special issue in the journal Frontiers in Public Health, this optimism often masks uncomfortable realities. The practice of science diplomacy has too often reproduced the very inequalities it aims to dismantle, operating within frameworks that privilege powerful nations and institutions while marginalizing voices from the Global South.

Lighting the Path: How the GlioLighT Consortium Is Exploring New Ways to Treat Brain Tumours
Across the world, scientists are still trying to answer one of medicine’s most difficult questions: how can we safely and effectively treat brain cancers such as glioma? Despite decades of effort, outcomes for people diagnosed with high-grade glioma remain bleak. Current treatments, including surgery, radiotherapy, and chemotherapy, can slow the disease, but rarely stop it. The GlioLighT consortium, a multidisciplinary European research team funded by the European Innovation Council, has come together to explore a novel approach based on direct light therapy. Being in a very early stage, the project doesn’t promise an immediate cure; instead, it sets out to answer a very fundamental question: can light itself trigger biological processes that might form the basis of a safe and targeted brain tumor therapy?

Prof. Vladimir Zharov | Detecting Malaria with Light and Sound Without Blood Draw Can Transform Global Health
For centuries, malaria has been one of the deadliest diseases on the planet. Nearly half of the world remains at risk of malaria with more than half a million deaths each year, most of them in children. While some progress has been made in controlling malaria and developing a vaccine, this has stalled recently, with a growing number of deaths since 2019. At the heart of the challenge is the lack of non-invasive and rapid diagnostic technologies for malaria, which are urgently needed, especially in remote or low-resource areas with limited healthcare infrastructure. Happily, a new frontier in medical technology is offering hope, in the form of the Cytophone, a revolutionary device that can detect malaria through the skin without drawing a single drop of blood. This innovation, developed by a team led by Prof. Vladimir Zharov at the University of Arkansas for Medical Sciences and licensed to Cytoastra for further commercialization, represents a leap forward not just in malaria diagnostics, but in how we might monitor disease altogether.

Dr. Jeffrey Curran Henson | When Lithium Slows the Heart, and How an unlikely Asthma Drug Offered a Way Out
For more than half a century, lithium has been one of the most reliable treatments for bipolar disorder. It has given countless people the ability to stabilize their moods and reclaim lives otherwise disrupted by cycles of mania and depression. But lithium comes with inherent risk: its therapeutic range is narrow, which means that the difference between a helpful dose and a harmful one is surprisingly small. Too much lithium in the body can lead to a cascade of health problems, including neurological confusion, tremors, kidney dysfunction, and, though much less well known, potentially dangerous effects on the heart. In a recent publication, Dr. Jeffrey Curran Henson of the University of Arkansas for Medical Sciences, and colleagues, shed light on one of lithium’s most alarming but underappreciated risks: its ability to disrupt the heart’s natural pacemaker, the sinus node. Their case study and systematic review tell the story of a patient whose life was threatened not by the mental illness she had long managed, but by the very medication that had allowed her to manage it. And in that story, the researchers also describe a novel way out: a treatment that avoided the need for invasive procedures and could reshape how we think about emergency care for lithium-related heart complications.

Speaking Science Across Languages: Rethinking Scientific Publishing in the Asia-Pacific
When we think about science, we often imagine a universal language of knowledge in the form of a shared code of numbers, graphs, and precise words that transcend borders. But what happens when the language of science is not the language of the scientist? This is the challenge explored in a recent study by a group of publication professionals from the pharmaceutical and medical communications industries across the Asia Pacific region. The study looked at how researchers in this region navigate the world of English-language scientific publishing. Their findings remind us that words matter, and the language we use can either invite voices into global conversations and knowledge exchange, or keep them out.

Dr. Kai Hilpert | AI-Powered Prediction of Antimicrobial Peptides in Human Serum: A New Strategy Against Resistant Bacteria
In the 20th century, antibiotics transformed medicine. Infections that once killed millions could be cured with a pill or injection. Surgeries became safer, cancer treatments more effective, and advanced medical interventions, such as organ transplants, became possible, all because doctors could rely on these drugs to control infections. Unfortunately, today, that foundation is crumbling. Bacteria are evolving faster than medicine can keep up. Common antibiotics are failing, and infections that were once easily treatable are becoming deadly again. In 2019 alone, antimicrobial resistance was linked to nearly five million deaths worldwide, making it deadlier than HIV or malaria. The economic cost is equally staggering: the World Bank warns of trillions lost in global productivity and millions pushed into poverty if nothing changes. This crisis, caused by antimicrobial resistance, has been described as a “silent pandemic.” Unlike a sudden outbreak, it spreads quietly, making routine medical care slightly more dangerous each year. Yet amid this grim outlook, new research is opening a window of hope. At the forefront of new innovations in this area are Dr. Kai Hilpert of City St George’s, University of London, and his colleagues, who are pioneering an approach that combines biology, chemistry, and artificial intelligence to reinvent how we discover infection-fighting medicines. Their work has been recognised with a prestigious award from the UK’s Biotechnology and Biological Sciences Research Council, BBSRC.
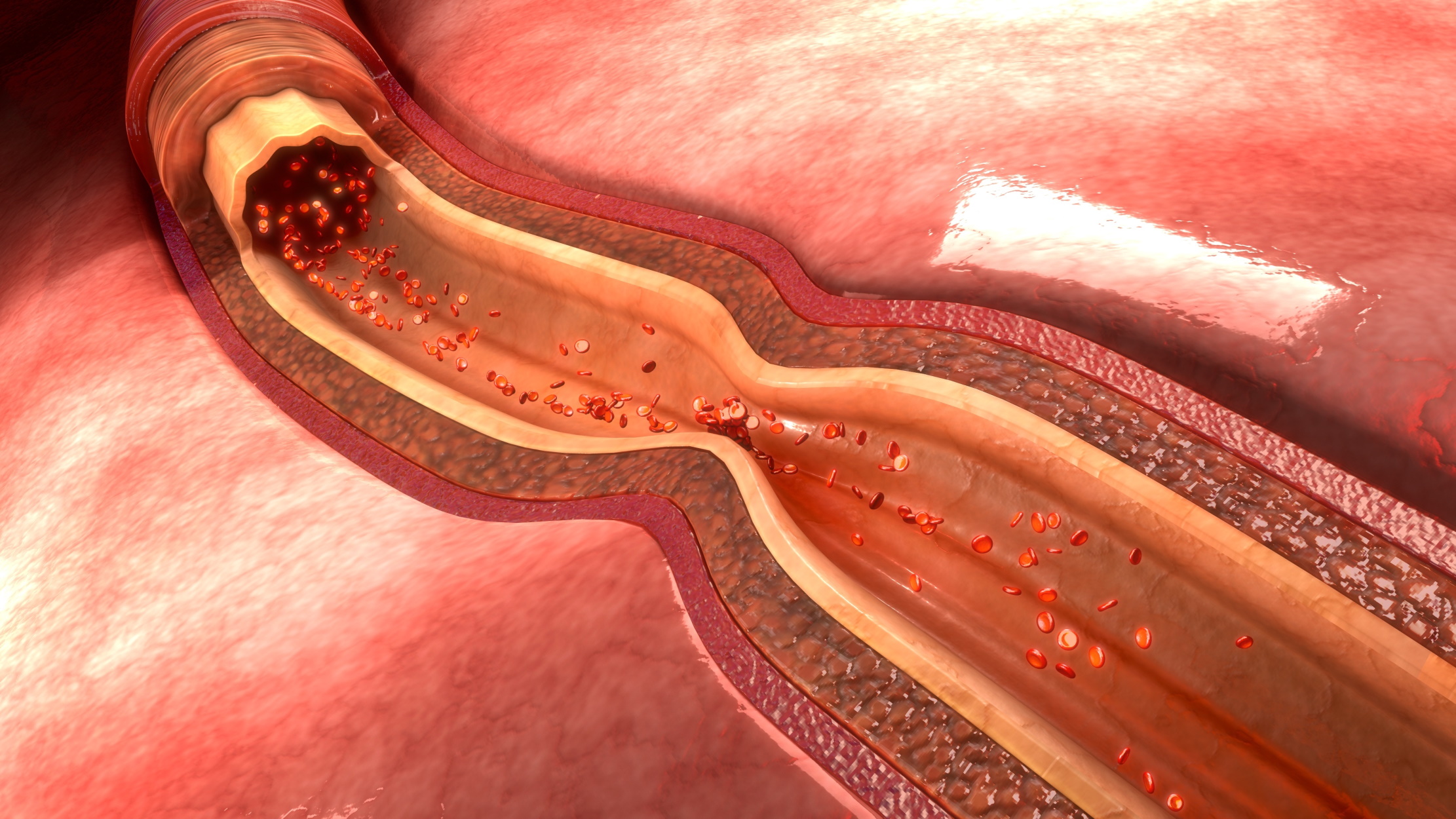
Dr Adrian-Sebastian Zus | When Arteries Rebel: Preventing Radial Artery Spasm
Most of us never give much thought to the small artery that runs along the inside of our wrist, the radial artery. You can feel it easily if you press your fingers just below your thumb. Yet in modern medicine, this little vessel has become one of the most important gateways to the heart. Imagine a doctor threading a tiny tube, called a catheter, through the radial artery to reach your heart. This technique, called transradial access, has transformed modern cardiology. By entering through the radial artery, doctors can perform life-saving cardiac procedures with fewer complications, faster recovery, and even lower costs than older methods that went through the leg. Many people can even walk out of the hospital on the same day. Over the past two decades, doctors have increasingly chosen the radial artery as their entry point for procedures like angiography (imaging of the heart’s blood vessels) and angioplasty (opening blocked arteries). But there’s a catch: sometimes the artery rebels. It tightens suddenly, almost like a muscle cramp, gripping the medical instruments and making the doctor’s job harder. This is known as radial artery spasm (or RAS for short). In rare cases, the spasm is so severe that it traps the catheter or damages the artery wall.

Professor Andrea Facciabene | Gut-Targeted Antibiotic Boosts Lung Cancer Radiation Therapy: A New Frontier in Microbiome-Based Treatment
Imagine a future where treating cancer doesn’t just depend on high-tech machines or potent drugs, but also on something as simple, and as complex, as the bacteria living in your gut. This future might be closer than we think, thanks to groundbreaking research led by Professor Andrea Facciabene at the University of Pennsylvania. In a randomized pilot study recently published in the Journal for ImmunoTherapy of Cancer, Prof. Facciabene and an international team of researchers explored a curious and compelling idea: could altering the gut microbiome enhance the effectiveness of radiation therapy in patients with inoperable early-stage lung cancer? The answer, at least in this early stage, appears to be yes.

The allure and pitfalls of flavored tobacco and nicotine products. Interview with Professor Mary Rezk-Hanna
Interview with Professor Mary Rezk-Hanna

Professor Dr. Frederik Wenz | McDonaldization in Healthcare: Opportunities and Pitfalls for Patients and Providers
If you stroll into a McDonald’s fast-food restaurant in Paris, Tokyo, or New York, you’ll notice that the Big Mac tastes the same, the menu looks familiar, and the process is quick and efficient. You order your food, wait a short while, and you get exactly what you expect. In the 1990s, American sociologist George Ritzer gave a name to this phenomenon: McDonaldization. He identified four principles behind the model’s success. The first is Efficiency, in terms of getting things done in the fastest, least expensive way possible. Second comes Calculability, which involves valuing numerical metrics, such as how many burgers sold and how fast they were served, over subjective qualities such as taste or ambiance. The third factor is Predictability, which involves making sure the experience is the same way everywhere. The final aspect is Control, where the corporation uses refined rules, technology, and systems to achieve the preceding three principles. While these ideas may work for burgers and fries, can they work if applied to something very different, such as healthcare? In a thought-provoking review, Professor Dr. Frederik Wenz of the University of Freiburg explores how these fast-food-inspired principles are transforming hospitals, clinics, and even the role of patients themselves. This phenomenon doesn’t just involve faster patient registrations or standardized treatments. It’s about a fundamental shift in how we think about healing, and how much responsibility patients are willing (or able) to take on themselves.